Part 1:
Gender-affirming care remains the evidence-based standard of care for gender dysphoria in transgender adolescents, despite claims by some laws and lawmakers that it is “experimental”.

AJ Eckert on June 25, 2022
In 2022 alone, fifteen states introduced a total of 25 bills intended to restrict access to gender-affirming (GA) care to trans children and adolescents. (“Trans,” a common abbreviation for “transgender,” is used here as an umbrella term to describe people whose gender identity does not align with the gender to which they were assigned at birth, and GA care includes medical, surgical, mental health, and non-medical care intended to affirm trans people in their gender identity.) Some of these bills even go so far as to criminalize GA care; for example, the Alabama law would make it a felony punishable by up to 10 years in prison for medical providers found “guilty” of prescribing gender-affirming puberty blockers and hormones to people under age 19. As a result of these legislative efforts, over 58,000 trans youth could potentially lose access to GA care, depending on how many become law and in which states.
The predominant theme of these bills is the claim that GA care is “experimental.” This false claim is commonly used as the primary justification for outlawing such care. Indeed, Arkansas, Louisiana, and Ohio bills even share the very same name, the Save Adolescents from Experimentation (SAFE) Act, and the preambles of many of these bills characterize GA care as not just experimental but harmful, while also making false scientific claims about biology, sex and gender, gender dysphoria, and the psychological and medical care of gender dysphoria. In this, these bills are reminiscent of the strategy that antivaxxers have used to demonize COVID-19 vaccines in which they portray them as “experimental” and therefore dangerous, even to the point of making false claims that these vaccines violate the Nuremberg Code.
For example, Ohio HB454, Arkansas HB1570, and Louisiana HB570 are bills that are essentially largely copy-and-pasted from each other, and all three state that the use of GA hormones in “biological females”—terminology that is inaccurate, as explained here—results in an increased risk of breast and uterine cancers. Evidence is limited for these claims. Indeed, in available studies, transmasculine people (assigned female at birth—or AFAB—people who are on gender-affirming testosterone) have been found to have, if anything, a lower risk of breast cancer and endometrial cancer and certainly no increased risk of ovarian cancer compared to cis women. This is just the start of the bad and cherry-picked science used in these bills to justify outlawing GA care.
The bills also state:
This assertion is, quite simply, untrue. A systematic literature review of research from 1991 to 2017 noted 52 studies showing overall improvement in the well-being of trans people following GA medical and/or surgical interventions, four studies showing mixed or null findings, and zero studies that GA interventions cause overall harm. More recent studies confirm that gender-affirming care can be immensely beneficial in properly selected candidates.The risks of gender transition procedures far outweigh any benefit at this stage of clinical study on these procedures.
Another common theme in these bills is the demonization of surgical procedures used for gender reassignment by at least implying—and often stating outright—that such surgeries are “genital mutilation” carried out on children. For example, Kansas SB214 would outlaw all “gender reassignment” surgeries for trans people under age 18 (the almost identical Idaho HB675 straight-out calls such surgeries “genital mutilation of a child”), exempting those youth with differences in sex development or who are intersex. To Kansas legislators, normalizing genitals is, apparently, more important than considering the harms of forced genital surgery. (Kansas lawmakers likely believe that making genitals look “normal” prevents “gender confusion”.)
Ironically, intersex surgeries are not medically necessary, while in contrast gender-affirming surgeries can be. In addition, GA bottom surgery (a colloquialism for genital and reproductive system surgeries, including phalloplasty, vaginoplasty, hysterectomy, and metoidoplasty) is rare before patients are of legal age to provide informed consent themselves.
Ignoring these facts, Alabama SB184 and HB266 nonetheless state:
There is a vast difference between gender affirmation and “aggressive pushing” of GA medical and surgical care. The latter description uses intentionally-fearmongering language that implies that doctors are somehow bullying children into transitioning and pushing their parents to provide consent for GA care. I would suggest that it is aggressive to outlaw and criminalize health care for those who are already marginalized. Additionally, once again it must be emphasized that genital surgery for gender reassignment is rarely carried out on patients with gender dysphoria who are under 18, intersex patients excepted.Some in the medical community are aggressively pushing for interventions on minors that medically alter the child’s hormonal balance and remove healthy external and internal sex organs when the child expresses a desire to appear as a sex different from his or her own.
The Alabama bill also claims:
Their parents are unable to comprehend? By that logic, we should outlaw everyone’s GnRH agonists, hormone therapy, and surgical procedures such as breast augmentation! Such is the quality of the arguments being made in support of these bills, right in the bills themselves!Minors, and often their parents, are unable to comprehend and fully appreciate the risk and life implications, including permanent sterility, that result from the use of puberty blockers, cross-sex hormones, and surgical procedures.
Experimental medicine
The argument that GA care is experimental is not new but continues to re-emerge and be used to argue against offering such care to minors. As Ari Drennen, LGBTQ program director for Media Matters for America, noted on Twitter:What makes a medical or surgical intervention “experimental”, though, as opposed to standard of care or an accepted option? The American Psychological Association defines an experimental treatment as “an intervention or regimen that has shown some promise as a cure or ameliorative for a disease or condition but is still being evaluated for efficacy, safety, and acceptability”. In general, experimental medical care and surgical procedures are not considered an acceptable standard of care for the treatment of the condition for which they are being evaluated and are generally still undergoing clinical trials to assess them for efficacy and safety. Some will be found in these clinical trials to be safe and effective, while most others will not and be abandoned.The new right wing angle of attack is that NO trans people should have access to hormone replacement therapy because it’s “experimental.” Trans people have literally taken cross-sex hormones since at least 1918. Governor DeSantis’ move is illegal, dangerous and based on lies.
Here I will argue that gender-affirming medicine is, by definition, not experimental, no matter how often it is characterized explicitly as such in bills introduced in Alabama, Arizona, Kansas, Louisiana, Missouri, Oklahoma, and Ohio. I will begin by discussing examples of medicine that is still considered experimental for comparison. After that, I will further break down the tenents of efficacy, safety, and acceptability for GA care.
There are many areas of health care that employ experimental medicine. Examples include gene therapy trials for cancer treatment, or the use of bacteriophages for bacterial infections. Experiments in medicine are necessary to advance the study of treatments and is widely accepted. In contrast to the use of the term “experimental” to describe such investigational treatments, in trans health care, the term “experimental” seems to be used exclusively as a derisive tagline to dismiss GA care. The intent behind this disparaging and dismissive use is to promote the view is that the safety and efficacy of GA care is so much in doubt that it cannot be generally used and requires more clinical trials to evaluate its efficacy and safety before it can be recommended. Of course, there is also a not-so-subtle implication behind labeling GA care “experimental”, namely that it is also dangerous, which then often leads to further claims that clinical trials of GA care would be unethical. In essence, those promoting these bills seem to be deceptively conflating experimental medicine (i.e., unproven treatments) with “disproven” treatments, safe in the knowledge that most people outside of medicine will not know the difference.
Let us move on to consider the efficacy and safety of GA care.
Efficacy of gender-affirming medicine
The World Professional Association for Transgender Health (WPATH), considered by many to be the leader in promoting evidence-based trans health care, has endorsed GA surgery and medical therapy to be effective and often life-saving care. The treatment efficacy of GnRHa in delaying puberty in trans youth has been thoroughly documented in scientific studies and publications since the 1990s. Studies support the conclusion that trans children supported in their gender identity by their families have rates of depression comparable to their cisgender peers. Studies suggest that youth that access gender-affirming care have improved body satisfaction and self-esteem, which is protective against poorer mental health and supports healthy relationships with parents and peers. Research consistently demonstrates that trans youth affirmed in their gender identity by their families have significantly better health outcomes. Moreover, social and medical gender affirmation is inversely related to mental health problems in trans people.Safety of gender-affirming medicine
It is essential to point out that puberty blockers, which are widely used to treat precocious puberty, seem only to be considered “experimental” and “dangerous” when used as part of GA treatment for pubescent trans youth. Some equate the use of off-label medications to experimental use of said medications. Off-label drug use is the common practice of prescribing an available medication for an indication that the FDA has not approved. Once medications are on the market, the FDA does not control or limit how health care providers prescribe them.Off-label use of gender-affirming treatment, such as puberty blockers in youth, does not make the treatment “experimental”. Again, GnRH analogs have been the gold-standard treatment in children with central precocious puberty since the 1960s and used in trans youth since the 1980s. When used in cis children, puberty blockers “have an enviable track record of safety and efficacy“. Puberty blockers are used similarly in trans youth once they hit puberty to halt permanent changes. It should be emphasized that the effects of blockers are both temporary and reversible.
Standard of care and gender-affirming medicine
One thing that nearly all standard of care treatments for any condition have in common is that they are recommended and endorsed by major professional societies after evaluation of existing evidence in the peer-reviewed medical literature by an expert panel. While those who seek to deny science-based medicine view this argument as an “appeal to authority”, an appeal to such an authority is not a logical fallacy when the authority is legitimate. Personally, I like to look at an appeal to expert consensus as nothing more than a convenient shorthand for referring to the existing evidence base. Moreover, general expert consensus statements from such medical societies always include lengthy discussions of the evidence, including strengths and weaknesses, upon which consensus recommendations are based, often also graded by the strength of the evidence supporting each recommendation.WPATH has been publishing standards of care (SOC) for trans health care since 1979, and GA care is endorsed by every major medical association. It is currently the standard of care for treating trans patients, be they an adult or adolescent. Contrary to a newly released and deeply flawed Heritage Foundation “study” that claims that access to GA care is associated with an increase in suicides (which was not even published in the peer reviewed medical literature), better quality research has consistently concluded that access to GA care can be lifesaving and improves mental health outcomes in trans youth. Indeed, trans youth thrive in supportive environments. Overall, the existing research base overwhelmingly supports an affirmative approach.
Indeed, even the American Medical Association (AMA)—definitely not a “woke” or even liberal organization—passed a resolution in 2008 supporting health insurance coverage for GA care of gender dysphoria that included the following passage:
The Dept. of Health and Human Services (HHS) has reaffirmed HHS support and protection of LGBTQ youth and has issued new guidance to clarify the topic of non-discrimination related to gender identity; as KFF.org, a ‘nonpartisan source of facts, analysis and journalism for policymakers, the media, the health policy community and the public,’ note:Health experts in GID, including WPATH, have rejected the myth that such treatments are “cosmetic” or “experimental” and have recognized that these treatments can provide safe and effective treatment for a serious health condition.
It is, quite simply, a misrepresentation of what a standard of care is in medicine and of what constitutes “experimental” medical interventions to argue that GA care is “experimental”. It is not. GA care is the current standard of care. That the evidence base is not as certain or settled as it is for, to cite examples, the evidence base supporting the current standards of care for various cancers, diabetes, hypertension, and the like does not make GA care for trans youth “experimental” any more than the same considerations make a lot of psychiatric care “experimental”. Moreover, that the standard of care will likely change in the future as new evidence accumulates does not make GA care now experimental, any more than the discovery that peptic ulcers are mainly due to bacteria (H. pylori) that can be well-treated with antibiotics rendered the past treatment of peptic ulcer disease somehow “experimental”.Specifically, the guidance states that categorically refusing treatment based on gender identity is prohibited discrimination under Section 1557. The guidance also states that Section 1557’s prohibition against sex-based discrimination is likely violated if a provider reports parents seeking medically necessary gender affirming care for their child to state authorities, if the provider or facility is receiving federal funding. The guidance further states that restricting a provider from providing gender affirming care may violate Section 1557.
Standards of care and clinical guidelines evolve and are regularly updated, which is why physicians have continuing education and board recertification requirements; it is imperative for us to stay on top of the latest available information. These evolving standards of care do not negate prior standards; both reflect the latest science-based evidence, and new standards of care supplant older ones as new evidence is accumulated. Indeed, new standards of care should supplant older ones based on evidence; if this were not the case, doctors would still be using bloodletting for nearly everything and commonly treating patients with concoctions that include cadmium and other toxic heavy metals.
Uncertainty in medicine
William Osler characterized medicine as “a science of uncertainty and an art of probability”.Opponents of trans care often point to the lack of randomized control trials of gender affirmation, ignoring that such trials would be near-impossible to carry out and often unethical. RCTs can show whether a treatment is better than a placebo. In application, however, carrying out an RCT in which one group of trans youth is randomized to GA treatment and the other to placebo is arguably unethical because there would not be clinical equipoise between the groups; i.e., genuine uncertainty about which group, control or experimental, would fare better or worse, which would suffer more harm or more benefit. Let me elaborate with an example. Where puberty blockers can stop distressing characteristics of an unwanted puberty from developing, withholding them from a control group would likely intensify feelings of distress, depression, anxiety, and dysphoria. Also, how does one randomize and double-blind an RCT in which the group receiving GA interventions will always feel the physical effects of treatment? We know that gender-affirming hormones cause physical changes (or, as with blockers, the lack of pubertal changes), while the placebo group will not show these changes. An RCT to demonstrate the efficacy of gender-affirming therapy is redundant.
RCTs are also very difficult to carry out in small, historically under-researched, and minoritized populations. As noted by a publication of the Symposium on Evidence Based Medicine:
Further, although RCTs are considered the gold standard of medical evidence, they are not infallible; for example, patients in trials are not always representative of patients in the real world.Small trials are methodologically challenging: the smaller a trial, the larger the treatment effect necessary for the results to be significant, so that it is easy to miss small effects that may be clinically, but not statistically, significant. Trials that show no statistically significant benefit are less likely to be published, and so less likely to make their way into systematic reviews and thus into the accepted evidence base. Other reasons why small studies that target disadvantaged populations are unlikely to be performed concern the funding of research and the comparative nature of many studies.
Upcoming research is evolving to include hard-to-reach and often omitted demographic groups and to work with instead of on trans people. There is a need for larger-scale studies that have questions about gender identity, notably absent in prior research, recruitment in rural areas as well as metropolitan, the inclusion of intersectional minorities overlooked and ignored by the system, and analysis of the specific factors that predict rejecting family behaviors and those that contribute to positive climates. Again, the existence of these gaps in our knowledge about who benefits most from GA care does not make GA care “experimental,” any more than uncertainty over which groups benefit most from different approaches to, for example, treating hypertension makes, for example, antihypertensive treatment “experimental.” People who are historically minoritized due to issues such as systemic racism have been excluded or underrepresented in studies on hypertension, aspirin use, diabetes, and cancer screening; further research will hopefully fill these gaps and inform new recommendations and guidelines. This does not make current hypertension guidelines, heart disease treatment and diabetes treatment, or preventive health measures “experimental”.
A closer look at some of the bills outlawing GA care
Trans Formations, a nonprofit “providing actionable information on harmful anti-trans legislation,” has detailed descriptions of all proposed, active, passed, and failed bills. The following are a few examples.Alabama’s recent Vulnerable Child Compassion and Protection Act (V-CAP) makes the provision of gender-affirming care to minors a Class C felony punishable by a $15,000 fine or up to 10 years in prison or both. Thankfully, a federal judge has issued a preliminary injunction to stop Alabama from enforcing the legislation. Unfortunately, the law includes an unblocked provision requiring schools to tell parents if their child discloses to a school official that they might be trans, putting those with unsupportive home environments at risk.
Texas Gov. Abbott and Attorney General Paxton recently moved to categorize gender affirmation for youth as child abuse and investigate and criminalize families who support their trans children in receiving age-appropriate gender-affirming care. A temporary injunction has halted the investigations. Yale Law School and Yale School of Medicine have issued a report examining the claims underlying the reasoning of the Texas bill and found both errors of omission and inclusion and that the medical claims were not grounded in reputable science.
Florida Gov. DeSantis’ administration is recommending to the Florida Board of Medicine that they ban gender-affirming care for minors and all Medicaid recipients, meaning a ban on all trans-related care for adults and minors on state insurance. This two-pronged tactic ensures quick action and avoids legislative approval. Last year, DeSantis signed the “Fairness in Women’s Sports Act“, a law preventing trans girls from competing on girls’ high school and college sports teams. He recently made a proclamation declaring a cisgender woman the “rightful winner” in the NCAA’s first division swimming championship won by transgender woman Lia Thomas, and in March, signed the colloquially-titled “Don’t Say Gay” bill (the “Parental Rights in Education” bill), that restricts education on gender identity and sexual orientation in public schools.
On June 2, Florida State surgeon general and secretary of the Florida Dept of Health Joseph Ladapo sent a letter to the Florida Board of Medicine recommending against not just surgical and pharmaceutical GA interventions for trans adolescents, but even non-pharmacological interventions. Ladapo has created prior controversy with his anti-mask stance, opposition to vaccine mandates, promotion of quack COVID treatments such as hydroxychloroquine, and an emergency rule that discriminates against Black farmers applying for medical marijuana licensure. He has also recommended against COVID vaccines for healthy children aged 5 to 17, making Florida the first state to do so formally. His recommendation was cherry-picked from three studies which in fact concluded that vaccines are safe and effective.
In his recent letter to the state medical board, Ladapo wrote:
Ladapo sources guidance released on April 20 by the Florida Dept of Health, which directly contradicts federal guidance by the HHS and has already been refuted by more than 300 Florida health care professionals, as well as the report of an investigation conducted by the Agency for Health Care Administration, which was released on June 2.As State Surgeon General, I recommended against certain pharmaceutical, non-pharmaceutical, and surgical treatments for gender dysphoria. The recommendations are based on a lack of conclusive evidence and the high risk for long-term, irreversible harms from these treatments…The current standards set by numerous professional organizations appear to follow a preferred political ideology instead of the highest level of generally accepted medical science. Florida must do more to protect children from politics-based medicine. Otherwise, children and adolescents in our state will continue to face a substantial risk of long-term harm.
The report summary, ironically titled “Let Kids Be Kids*”, has been condemned by WPATH and the United States Professional Association for Transgender Health (USPATH), which had also previously debunked research cited in the April 20th guidance.
*writer’s note: unless they’re trans.
Prevent Child Abuse America, “the nation’s oldest and largest organization committed to preventing child abuse and neglect before it happens“, issued a statement reacting to the Texas AG’s opinion and in support of gender-affirming care:
Regardless of the outcomes on a state and federal level, the current political debates have detrimental consequences. The Trevor Project’s National Survey on LGBTQ Youth Mental Health 2021 found that recent politics negatively impacted 94% of LGBTQ youths’ mental health. South Dakota was the first state to enact an anti-trans bill in 2022; 90% of LGBTQ youth in South Dakota are diagnosed with depression or anxiety.Prevent Child Abuse America (PCA America) knows that providing necessary and adequate medical care to your child is not child abuse and that transgender and non-binary children need access to age-appropriate, individualized medical care just like every other child.
As Adm. Rachel Levine, MD, U.S. Assistant Secretary for Health, has stated:
In addition, trans people are more than four times as likely as cis people to be victims of violence and inadequate police and legal protection. 74 elected law enforcement leaders and prosecutors summed up the criminalization of GAM in a joint statement:Trans youth in particular are being hounded in public and driven to deaths of despair at an alarming rate. Fifty-two percent of all transgender and nonbinary young people in the U.S. seriously contemplated killing themselves in 2020. Think about how many of them thought it was better to die than to put up with any more harassment, scapegoating and intentional abuse.
Bills that criminalize safe and crucial medical treatments or the mere public existence of trans people do not promote public safety, community trust, or fiscal responsibility. They serve no legitimate purpose…we do not support the use of scarce criminal justice and law enforcement resources on criminalization of doctors who offer medically necessary, safe gender-affirming care to trans youth, parents who safeguard their child’s health and wellbeing by seeking out such treatments, or any individuals who use facilities aligned with their gender identity.
Conclusion: Politicians should not dictate medical care
Bills cannot claim to protect kids while harming them. Medical experts support gender-affirming care; politicians should not be interfering in medical decisions made between a health care provider and their patients. Contrary to the rationale used to justify bills outlawing GA care in adolescents and making such care more difficult for adults to access, even with the uncertainties in the evidence base for treating gender dysphoria and trans youth, GA care is not experimental. Rather, it is the standard of care. Laws seeking to ban GA care are no more science-based than laws seeking to make ivermectin available over-the-counter to treat COVID-19, to limit school vaccine mandates, or to license naturopathy and other pseudomedicine. They are, as recently retired SBM editor Jann Bellamy used to like to describe laws legalizing pseudomedicine, legislative alchemy.Source (Archive)
Part 2:
A lot of the “facts” about providing healthcare to transgender youth turn out to be not actually facts. We present here a summary of the evidence relating to transition-related health care for transgender adolescents.

Brynn Tannehill on July 3, 2022
Currently, several states in the U.S. are moving to ban transgender youth from accessing gender-affirming (GA) care. Three days after the Supreme Court overturned Roe v. Wade, Alabama cited the decision as support for a law that makes GA care for youth, including puberty blockers and hormones, a felony. Alabama, Arkansas, and Arizona have current laws banning or restricting gender-affirming care for youth. As MSNBC Opinion Columnist Katelyn Burns has observed, trans youth appear be at ground zero in the conservative culture war. In a Pew Research Center survey of 10,188 U.S. adults, 46% supported making gender-affirming health care illegal for those under 18. A new NPR/Ipsos poll found that 14% of Democrats and 55% of Republicans support state laws that prevent trans youth from accessing gender-affirming care.'
GA medicine is the standard of care as acknowledged by all major medical associations. Part I of this series established that GA care is not experimental. In Part II, author and transgender advocate Brynn Tannehill presents, along with Dr. A.J. Eckert and SBM managing editor Dr. David Gorski, what is currently known about science-based GA care. This post will take the form of, in essence, bullet points answering false and misleading claims commonly used to attack GA care for trans adolescents. The answers are not comprehensive, as this list is intended as a useful reference. We might in the future publish more detailed posts addressing specific questions summarized below.
Affirming treatment for transgender youth follows the internationally recognized standards of care
Puberty suppression for trans youth is the standard of care set forth by the Endocrine Society and the World Professional Association of Transgender Health (WPATH), which represents the global consensus on transgender healthcare.Social transition for pre-pubertal youth improves mental health outcomes
A 2016 study of socially transitioned trans youth between the ages of 6-14 had mental health similar to their peers. This study included a cisgender control group, along with siblings of the trans youth. Transgender children reported depression and self-worth that did not differ from their matched-control or sibling peers, and they reported only marginally higher anxiety (p = .076). These findings are in striking contrast to previous work with gender-nonconforming children who had not socially transitioned, which found very high rates of depression and anxiety. A 2018 meta-study concluded that “Newer research suggests that socially transitioned prepubertal children are often well adjusted, a finding consistent with clinical practice observations”.Stigma, discrimination, and lack of familial acceptance are predictors of adverse mental health outcomes for transgender youth. Conversely, acceptance is predictive of positive outcomes
Numerous studies have found that stigma, discrimination, and lack of familial acceptance are predictors of poor mental health outcomes for trans youth. A 2017 study of stigma and discrimination found that both were predictors of self-injury, suicide, depression, and anxiety among a sample of 923 Canadian transgender 14- to 25-year-old adolescents. Other studies have found that discrimination, stigma, and bullying are the driving factor behind negative outcomes for youth who are otherwise supported at home. Another found that minority stress was associated with major depressive disorders and anxiety disorders. Another 2020 study found that interpersonal and environmental microaggressions, internalized self-stigma, and adverse childhood experiences (ACEs), and protective factors: school belonging, family support, and peer support affected lifetime recalled suicide attempts and suicidality over the past six months.Acceptance at home and at schools is predictive of positive outcomes. A 2019 study found that using chosen names associated with large reductions in negative health outcomes and improvements in positive mental health outcomes. A quantitative 2016 study found that parental closeness was related to significantly lower odds of all four mental health outcomes measured, and intrinsic resiliency positively reduced risk for psychological stress, PTSD, and stress related to suicidal thoughts. Trans youth are far more likely to be abused or rejected by their families than their cisgender peers, which results in worse mental health outcomes.
GnRH analogs (puberty blockers) have been FDA-approved for use for minors in the US since 1993
Doctors prescribe drugs which block the onset of puberty in order to give the child’s brain time to mature, to allow for exploration of gender identity, and to avoid an incongruent puberty. Contrary to frequent claims by “gender critical” activists, these drugs are not prescribed for prepubertal children; indeed, these drugs are not prescribed until Tanner Stage II of puberty, which is the onset of secondary sex changes. The most commonly used puberty-suppressing drugs in youth are Gonadotrophin-releasing hormone agonists (GnRHa) such as leuprolide. They have been FDA-approved to prevent precocious (early onset) puberty since 1993.Treating adolescents with gender dysphoria with puberty suppressing medications is not experimental
GnRHa was first used in the treatment of gender dysphoria in 1988, and its use for this purpose has been common since the mid-1990s. The Royal College of Psychiatrists, in 1998, recommended delaying puberty as the standard treatment in adolescents who experienced strong and persistent ‘cross-sex identification’ and distress around the physical body that intensifies with the onset of puberty. Similarly, the WPATH standards of care since the 1990s (WPATH Standards Of Care For Gender Identity Disorders—Fifth Version) have recommended blockers as the standard of care for dysphoric adolescents entering Tanner Stage II of puberty. When the US District Court for the Middle District of Alabama looked at the question of whether blockers and gender-affirming hormones for trans youth are experimental, it concluded:Similarly, as discussed in Part I, off-label use does not mean “experimental”.Defendants produce no credible evidence to show that transitioning medications are “experimental.” While Defendants offer some evidence that transitioning medications pose certain risks, the uncontradicted record evidence is that at least twenty-two major medical associations in the United States endorse transitioning medications as well-established, evidence-based treatments for gender dysphoria in minors.
Gonadotrophin-releasing hormone agonists (GnRHa) and hormone replacement are regarded as generally safe for adolescents by the Endocrine Society
Several studies have examined concerns about puberty suppression. A 2020 study found that suppression does not have an effect on cognitive functioning. Others have looked at those treated with GnRHa for precocious puberty and found that “[bone mineral density was] recovered within 1 year after GnRHa treatment discontinuation, and there were no abnormalities in reproductive function”. It also found that “bone mineral density decreases during GnRHa treatment, but recovers to normal afterwards, and peak bone mass formation through bone mineral accretion during puberty is not affected”. Long term follow up with the patient from 1988 found normal bone mineral density. Though there is a decrease in bone density while on them, the risk of fracture is still very low.Henriette Delemarre-van de Waal, MD, PhD of the Endocrine Society concluded her 2013 study on the safety and efficacy of puberty suppression by stating:
Other studies found minimal risks for 16-17 year old youth who began hormone replacement therapy. A 2022 meta-study of bone density in transgender people, including blockers and gender-affirming hormones concluded that, “Gonadotropin-releasing hormone (GnRH) analogues in transgender youth may cause bone loss; however, the addition of GAHT restores in both transboys and transgirls.” It also found that, “GAHT (including blockers) does not have a negative effect on BMD (Bone Mineral Density) in adult transwomen and transmen.”Hormonal interventions to block the pubertal development of children with gender dysphoria are effective and sufficiently safe to alleviate the stress of gender dysphoria.
It is worth noting that the side effects of any drug must be weighed against the harms of non-treatment, which in the case of transgender youth are likely to be significant and permanent.
Puberty suppression is considered fully reversible
The Endocrine Society’s Clinical Practice Guidelines (i.e. standards of care) states:Pubertal suppression is fully reversible, enabling full pubertal development in the natal gender, after cessation of treatment, if appropriate.
The vast majority of trans adolescents are competent to make medical decisions
Clinicians have standardized psychological tools to assess the competence of patients, whether they are cisgender or transgender. This is the standard by which it is determined whether individuals can give informed consent. In a 2021 study, clinicians applied the MacArthur Competence Assessment Tool for Treatment (MacCAT-T) to 74 trans adolescents between the ages of 10-18. The MacCAT-T tests found that 89.2% were competent. This test agreed with physician assessments 87.8% of the time. It is worth noting that mental health professionals and physicians are always expected to evaluate patients’ ability to give informed consent.In addition, although laws and conditions vary, a number of US states allow minors between the ages of 13 and 17 to give informed consent for certain medical procedures and treatments under the mature minor doctrine. Eight states have conditional age limits higher than 14 for people to legally consent to certain medical procedures and treatments, with the conditions usually involving whether the minor is emancipated and the nature of the condition for which medical treatment being sought (e.g., infectious disease, mental health, reproductive health). In the remaining states (plus D.C.) it is possible for unemancipated minors under specific conditions to consent to routine medical procedures,
Every major medical and mental health professional organization in the US supports access to transition-related care
Twenty-nine major professional health organizations have recognized the medical necessity of treatments for gender dysphoria and endorse such treatments. Most of these groups have also explicitly rejected insurance exclusions for transgender-related care, and few of these could be considered in any way “liberal” organizations (in the case of, for example, the AMA, quite the opposite, in fact). These include:| American Academy of Child and Adolescent Psychiatry | American Nurses Association |
| American Academy of Family Physicians | American Osteopathic Association |
| American Academy of Nursing | American Psychiatric Association |
| American Academy of Pediatrics | American Psychological Association |
| American Academy of Physician Assistants | American Public Health Association |
| American College Health Association | American Society of Plastic Surgeons |
| American College of Nurse-Midwives | Endocrine Society |
| American College of Obstetricians and Gynecologists | National Association of Nurse Practitioners in Women’s Health |
| American College of Physicians | National Association of Social Workers |
| American Counseling Association | Pediatric Endocrine Society |
| American Heart Association | Society for Adolescent Health and Medicine |
| American Medical Association | World Medical Association |
| American Medical Student Association | World Professional Association for Transgender Health |
Medical organizations supporting restrictions on access to health care are nearly universally small, religiously-based outfits, whose positions on LGBT issues are founded on religious beliefs rather than evidence-based medicine.
A large body of evidence demonstrates the benefits of treatment for transgender youth
Decades of research and dozens of studies have shown that access to treatment to delay puberty, followed by hormone therapy, has a beneficial effect for transgender youth: see de Vries (2014), Costa (2015), and Lara (2020). A 2020 study of transgender adults who had received treatment as youth found that “pubertal suppression for transgender adolescents who want this treatment is associated with favorable mental health outcomes.” Head author of the study, Dr. Jack Turban, concluded that the findings add to a “growing evidence base suggesting that gender-affirming medical care for transgender youth is associated with superior mental health outcomes in adulthood”. A 2021 meta-analysis of 9 qualifying studies (one which was considered “excellent” quality, five considered “good”) on the effects of GnRHa found that the common benefits among them were decreased suicidality in adulthood, improved affect and psychological functioning, and improved social life. A study released in December 2021 compared two groups of transgender youth: those who wanted Gender Affirming Hormone Therapy (GAHT) but did not receive it, and those who wanted and received it. The study found that those who received GAHT had lower odds of recent depression and of a past-year suicide attempt.A comprehensive literature review of 16 studies examining the benefits of puberty blockers and gender-affirming hormones in trans youth revealed that 13 of the 16 showed blockers and hormones resulted in statistically significant improvements in mental health, and none of them showed a decline. Two of these three studies found an improvement, but it did not reach the level of statistical significance due to small sample sizes. A 2022 study found that access to transition-related care, including blockers and hormones, was associated with 60% lower odds of moderate or severe depression and 73% lower odds of suicidality over a 12-month follow-up. A 2020 longitudinal study of access to blockers and gender-affirming hormones found that youth depression scores and suicidal ideation decreased over time while mean quality of life scores improved over time when given access to these treatments.
Some studies even indicate mental health outcomes for transgender youth who have undergone treatment is equal to their cisgender peers
A 2020 study compared the psychological health of 272 adolescents who had been referred for assessment for gender dysphoria at Amsterdam’s VU University Medical Center and had not yet received puberty blockers or hormones, and 178 adolescents who had been diagnosed with gender dysphoria and were taking puberty blockers but had not started hormone therapy. Those who hadn’t received any treatment had higher (worse) scores on measures of internalizing problems, suicidality, and problems with peer relations than the group receiving puberty blockers and a group of cisgender (non-transgender) controls. However, the group taking puberty blockers showed no differences in self-harm or suicidality compared to the cis control group, and even scored lower (better) than cis controls for internalizing problems.Other studies have found the same. In 2015 a study found that the combination of psychological support and puberty-delaying medication enabled subjects to reach levels of psychosocial functioning comparable to peers. A 2014 study in the Netherlands found that psychological functioning steadily improved over the course of the study and by adulthood these now-young adults had global functioning scores similar to or better than age-matched peers in the general population. More recently a study of trans youth in Spain found the transgender adolescents at baseline had worse measures of mental health than the cisgender control adolescents but that this difference equalized by the end of the study.
It must be noted that achieving results equal to the matched control group is the best possible outcome in mental health care.
There is no evidence that access to transition-related medical care causes harm
Opponents of gender-affirming medical care for transgender people often point to a study by Celia Dhejne as evidence that transgender people do worse if given access to care. However, the study does not say this: in fact it only shows that suicide rates for transgender individuals in Sweden who had surgery prior to 1989 were higher than the general public. It does not show that rates are higher for transgender people who have surgery than those who do not. Dr. Dhejne, lead author for the paper, has gone on record stating that her research cannot (and should not) be used to reach a conclusion that medical care for transgender people is harmful.Cornell University conducted a systematic literature review of all peer-reviewed articles published in English between 1991 and June 2017 that assess the effect of gender transition on transgender well-being. They identified 55 studies that consist of primary research on this topic, of which 51 (93%) found that gender transition improves the overall well-being of transgender people, while 4 (7%) report mixed or null findings. None found that transition was harmful.
While access to medical care has not been shown to harm transgender people, risk factors for suicidality among transgender people include lack of access to non-surgical medical affirmation. Other key factors are family rejection and lack of government recognition of their identity.
Double blind and randomized control trials (RCT) on healthcare for trans youth are not ethical or feasible
Many opponents of GA health care for trans youth, and even for adults, point out that the studies generally cited to support such care do not meet the “gold standard” of being double blind and RCT. This is an impossible burden of proof for this clinical question for multiple reasons. First, double-blind studies involving blockers or gender-affirming hormones are at least not feasible and, actually, impossible given that both the doctor and the patient will notice whether puberty has not continued (if on blockers alone), or if gender-affirming hormones are causing the patient to develop secondary sex characteristics, such as facial hair, deepening voice, or increased breast tissue.As for RCT, there is consensus in the field that such a trial would be unethical given the body of literature we have so far indicating that those in the control group would be likely to suffer adverse mental health outcomes compared to those randomized to the treatment groups. For this reason no Institutional Review Board would approve a randomized controlled trial at this time, because there would not be clinical equipoise, the requirement that there be genuine uncertainty based on science and previous clinical studies as to which group in an RCT will do better. Clinical equipoise is a minimum prerequisite for an RCT to be considered ethical.
Trans youth who have had medical treatment have significantly better mental health outcomes than those who do not
While RCTs are not feasible, comparisons of youth receiving treatment and those who haven’t have been done using convenience samples. A 2018 study of young transgender men who underwent chest reconstruction found their mental health was significantly better than the control cohort who were denied the surgery. A 2019 study of 47 trans youth before and after receiving hormone therapy found that the hormone therapy improved their mental wellbeing. It also found that those who had received puberty blockers for some time prior to hormone therapy ultimately reported even lower suicidality than those who had not previously received puberty blockers. In the largest study of this to date, researchers compared 272 transgender adolescents referred to the gender clinic who had not yet received pubertal suppression with 178 transgender adolescents who had received pubertal suppression. They found those who received pubertal suppression had better mental health outcomes than those who did not receive pubertal suppression. A study released in December 2021 compared two groups of transgender youth: those who wanted Gender Affirming Hormone Therapy (GAHT) but did not receive it, and those who wanted and received it. The study found that those who received GAHT had lower odds of recent depression and of a past-year suicide attempt.Long term follow-up found a similarly positive outcome for transgender adults who had followed the protocol as youth
Dutch researchers who studied young adults over the age of 18 who had followed the protocol of blockers followed by gender-affirming hormones found:Gender Dysphoria (GD) was alleviated and psychological functioning had steadily improved. Wellbeing was similar to, or better than, same-age young adults from the general population.
Desistance and detransitioning are rare after the onset of puberty
The Royal Children’s Hospital Gender Service in Victoria began treating transgender youth in 2003 and has taken in 701 patients for assessment. The court found that 96% of all youth who received a diagnosis of Gender Dysphoria from 2003 to 2017 continued to identify as transgender or gender diverse into late adolescence. No patient who had commenced gender-affirming hormones had sought to transition back to their birth assigned sex. Similarly, de Vries’ long term study of trans youth did not find any pattern of detransition or regret. Nor did a study of 75 German trans youth have any who expressed regret. A 2020 study of 143 Dutch transgender youth who started blockers found only 5 (3.5%) ended up discontinuing gender-affirming treatment. A 2022 retrospective review of Spanish trans minors found that out of a sample of 124 diagnosed with gender dysphoria, 97.6% persisted over a period of 2.6 years (on average). Prior to the first meeting, 48.5% were living in their affirmed role and, by the end of the study, this percentage rose to 87.1%. A long term (5 year) study of 317 trans youth (average 8.1 years) who socially transitioned found that most youth identified as binary transgender youth (94%), including 1.3% who retransitioned to another identity before returning to their binary transgender identity. 3.5% identified as nonbinary, and only 2.5% identified as cisgender.Further, UK GIC clinicians conducted a records review of 3,398 transgender patients at the Charing Cross, Tavistock, and Portman clinics. They found only two (.06%) who had detransitioned due to regret or deciding that they were not actually transgender. Similarly, a Dutch study of 6,793 patients who medically transitioned found only 7 (.1%) who regretted transition because they decided they were not transgender. Among those few adolescents who detransition, including those who have undergone hormonal interventions, research indicates that most do not regret having been given the opportunity to explore their gender. A 2021 study of youth who ceased puberty suppression found that many were glad to have had puberty suppression available because it safely offered them time and space to explore their gender identity.
Regret among those trans teens undergoing chest reconstruction is also rare. The most recent study found that less than 1% of trans men who had chest reconstruction before the age of 18 had regrets. Conversely, approximately 5% of cisgender women who undergo breast reduction experience regret, and this is considered by plastic surgeons to be extremely low.
The “watchful waiting” model does not suggest withholding medical care for transgender youth
Most clinicians caring for transgender youth in the UK use the “watchful waiting” approach. This approach has been described by the Center for Expertise on Gender Dysphoria in Amsterdam, the first clinic to offer gender-affirming medical interventions for transgender adolescents. The approach involves waiting until transgender youth reach puberty before recommending that they socially transition (i.e. start living with a name, pronouns, clothing, etc. that match their gender identity). This approach is only about prepubertal children, who do not receive medical interventions under any clinical guidelines. The watchful waiting approach is irrelevant to the discussion of medical interventions for transgender youth. Under existing guidelines, these interventions are never offered before the onset of puberty.Available evidence does not show puberty suppression causes transgender identity to persist
A 2015 qualitative study of clinicians and pediatric endocrinologists who administer puberty suppression to both transgender and cisgender youth asked the question: does puberty suppression disrupt the formation of gender identity? They noted that none of them had observed puberty suppression to cause dysphoria in youth with precocious puberty. Most of the endocrinologists in the study emphasized that they deliberately start treatment with puberty suppression only when the transgender youth have ‘…reached Tanner stage two or three to give them at least a kind of “feeling” with puberty before starting with puberty suppression,’ to avoid the possibility of steering.The standards of care recognize the overwhelming consensus that if a youth still has a strong transgender identification after the onset of puberty, it is unlikely to change, and beginning the puberty suppression protocol is likely the best course of action to gain time for further assessment and prevent potential irreparable harms. Dr. Kenneth Zucker, the researcher most associated with the early studies that 80% of youth desist, has himself acknowledged in an interview:
The more plausible, and generally accepted explanation among those who treat transgender youth is that standards and clinicians have become better over time at identifying youth who are genuinely transgender. In 2013 the DSM-5 changed the diagnostic criteria for transgender youth to require, “clinically significant distress or impairment related to a strong desire to be of another strong cross gender identification,” for a gender dysphoria diagnosis, rather than just gender nonconforming expression, interests, or activities. Similarly, researchers have known for almost a decade what factors are most predictive of continued trans identity into adulthood.… in adolescence the most likely outcome is the persistence of gender dysphoria… The treatment would be social transition and biomedical treatment.
Delaying transition until adulthood is likely to do lasting and irreparable psychosocial harm
A 2006 study by the pioneers of the Dutch Protocol for treating minors noted:Another follow-up study concludes:Physical treatment outcome following interventions in adulthood is far less satisfactory than when treatment is started at an age at which secondary sex characteristics have not yet been (fully) developed… [They] Often have difficulties in connecting socially and romantically with peers while still in the undesired gender role, or the physical developments create an anxiety that limits their capacities to concentrate on other issues.
A clinical study published in 2020 compared the outcomes of youth who started medical transition at various points, and found:Nonintervention is not a neutral option, but has clear negative lifelong consequences for the quality of life of those individuals who had to wait for treatment until after puberty.
More recent studies have shown that trans youth receiving treatment have better mental health, and specifically recommends against delaying treatment in order to prevent unnecessary mental anguish and potential permanent harm. The largest sample size study on this subject shows that trans people who began treatment prior to the age of 18 have a significantly lower lifetime risk of suicide attempts. Another study found that youth who had appearances less congruous with their gender identity (caused by treatment delays) were much more likely to suffer from major depressive disorders. A 2021 analysis comparing the results of similarly structured studies in Canada, Switzerland, England, and Australia found that prompt access to gender-affirming care was crucial to ensuring and improving the well-being of the young people who sought it. It was generally found that those who were prevented from prompt access to care self-reported mental health difficulties more often than those who had ready access to care.Older age and late pubertal stage are associated with worse mental health among Gender Incongruent (GI) youth presenting to Gender Affirming Medical-Care (GAMC).
Treatment decisions for minors are made based on input from parents, psychologists, psychiatrists, and the adolescent
The decision of whether to administer puberty blockers are not made solely by the child. In practice, a team of specialists evaluates each case extensively before making any decisions about treatment. The youth Gender Clinic in the Netherlands, which the Tavistock’s protocols are based on, describes an assessment process involving the adolescent, their parents, psychologists, and psychiatrists. The GeMS clinic for trans youth at Boston Children’s Hospital also includes parents, psychologists, psychiatrists, social workers, and endocrinologists as part of a comprehensive diagnostic process. WPATH, The Endocrine Society, and bioethicists who have studied the issue, consider 12-13 year-olds capable of giving informed consent to a fully-reversible treatment. Other bioethicists who have looked at the issue have concluded:…the available scientific evidence does not corroborate the view that adolescent medical transition is dangerous. Consequently, adolescent medical transition should be recognized as ethical and remain available. (from Ashley, F. (June 2022) Adolescent Medical Transition is Ethical: An Analogy with Reproductive Health, Forthcoming in Kennedy Institute of Ethics Journal)
Rapid Onset Gender Dysphoria (ROGD) is not an actual diagnosis
In 2018 Dr. Lisa Littman published an article alleging that transgender identities in youth are a form of social contagion. The article suffered numerous methodological flaws. Dr. Joshua Safer, Spokesman for the Endocrine Society stated that:As a result, it was partially retracted with corrections, and the publisher issued an apology. WPATH has put forward the following statement on the subject:Littman has actually written a paper about the anxiety of parents who question an open approach to transgender care and who frequent [web]sites that cast doubt on the current management approaches. No children were involved.
The term “Rapid Onset Gender Dysphoria (ROGD)” is not a medical entity recognized by any major professional association, nor is it listed as a subtype or classification in the Diagnostic and Statistical Manual of Mental Disorders (DSM) or International Classification of Diseases (ICD). Therefore, it constitutes nothing more than an acronym created to describe a proposed clinical phenomenon that may or may not warrant further peer-reviewed scientific investigation.
Higher quality follow up clinical studies have disproven the ROGD hypothesis
Following Littman’s proposed RODG diagnosis, several follow-up studies in clinical settings examined her hypotheses. In both studies involving controlled environments with higher quality data involving both trans youth and their parents, they found the opposite of what Littman suggested. First, a study on whether gender dysphoria onset was rapid found that transgender youth typically wrestled with gender dysphoria for years before coming out to their parents. It also found that parents understanding of their children was often flawed, and generally lagged behind the adolescent’s understanding of themselves. The paper proposed a better model, substantiated by data provided by parents and youth, for how the coming out process works.
A second clinical study attempted to verify Littman’s proposed causes for the emergence of gender dysphoria. The study noted:
The study’s conclusions supported the earlier conclusion that parents’ perceptions of dysphoria onset were incorrect, and that dysphoria drives anxiety and depression, not the other way around:…a distinct pathway of rapid onset gender dysphoria was recently hypothesized based on parental data. Using adolescent clinical data, we tested a series of associations that would be consistent with this pathway, however, our results did not support the rapid onset gender dysphoria hypothesis.
A second study reached a similar conclusion that trans youth generally wait months or years before coming out to their parents, resulting in the revelation seeming sudden to parents, but a long-held secret to the child.We did not find support within a clinical population for a new etiologic phenomenon of rapid onset gender dysphoria during adolescence. Among adolescents under age 16 years seen in specialized gender clinics, associations between more recent gender knowledge and factors hypothesized to be involved in rapid onset gender dysphoria were either not statistically significant, or were in the opposite direction to what would be hypothesized. This putative phenomenon was posited based on survey data from a convenience sample of parents recruited from websites and may represent the perceptions or experiences of those parents, rather than of adolescents.
Children are not being rushed into transitioning
Two years ago, the wait time for a youth appointment at the UK’s Tavistock Gender Identity Clinic was over a year. Today, that wait time has risen to over two and a half years. For adults in the UK’s national health system, the wait is now 33-36 months. For a youth to be seen, there must have been a year or more of gender incongruence. There are cases of youth waiting so long that they age out and must start all over again on the adult waiting lists. Other previously cited studies show that teens generally take many months or years before coming out to their parents and seeking treatment.The number of youths assigned female at birth being diagnosed with gender dysphoria is not disproportionate to the expected transgender population
A 2017 UCLA report, based on CDC survey data, states that 0.7% of youth aged 13-17 in the United States identify as transgender. This figure suggests that 700 in 100,000 youth born female may be transgender. As of 2019, Tavistock reports 1,740 patient referrals who are assigned female at birth. Assuming that there are roughly 6 million females in the UK between the age of 3 and 18 (the age range for Tavistock youth clinic services), only 29 in 100,000 of girls between 3 and 18 are referred for evaluation. This is indicative that there are potentially many youth who identify as transgender, and would benefit from treatment, still not being seen. It does not support the narrative that a large number of youth who are not transgender are availing themselves of Tavistock’s services.Tavistock reports the number of new cases of trans youth has levelled off
Despite concerns that the increasing number of cases is due to some form of social contagion, the number of youth being referred is still relatively small compared to the expected number, and has levelling off based on Tavistock’s own numbers.Bell v. Tavistock was overturned on appeal
Opponents of access to transition related care for minors frequently cite the case of Bell v. Tavistock in the UK. They neglect to mention that the initial decision was overturned by a higher court, which found that, “it is for the clinicians to exercise their judgement knowing how important it is that consent is properly obtained according to the particular individual circumstances”.The connection between autism and transgender identity remains speculative and does not affect the standards of care
Some studies suggest a link between autism and gender dysphoria. Others have looked at the same data and found no link when accounting for other factors. It is also worth noting that just because someone is autistic does not mean that they cannot be transgender, and there is no extant evidence that trans youth with ASD do not benefit from affirming care the same way neurotypical youth do.Attempts to change a person’s gender identity are both harmful and ineffective
A 2019 study looked at the long-term harms of conversion therapy on transgender youth. It found that adult transgender people who had been subjected to conversion therapy as minors were more than twice as likely to have attempted suicide over their lifetime. This relationship held true whether the therapy was religious or secular. The WPATH Standards of Care state that “Treatment aimed at trying to change a person’s gender identity and expression to become more congruent with sex assigned at birth has been attempted in the past without success, particularly in the long term. Such treatment is no longer considered ethical.” A 2022 study in Korea found that transgender individuals who had undergone conversion therapy were at much higher risk of depression, panic disorders, and suicide attempts.Transition is not a form of conversion therapy
Conversion therapy is an attempt to change or suppress a person’s sexual orientation or gender identity. Sexual orientation is an enduring pattern of romantic or sexual attraction to persons of the opposite sex or gender, the same sex or gender, or to both sexes or more than one gender. In other words, sexual orientation is who you are attracted to.Transitioning does not attempt to change who a person is attracted to, and thus is not a form of conversion therapy. The fact that the label for their attractions may change when a person transitions does not make transition a form of conversion therapy.
There is no evidence to suggest that trauma causes people to be transgender
A recent academic post online that has gained attention suggests (without citation) that trauma causes youth to have transgender identities, and that therapy to resolve these issues will cause them to desist in a transgender identity. This model, and the treatment proposed, is not significantly different from the that proposed by foremost proponents of sexual orientation “conversion” or “reparative” therapy in the United States. Entering therapy, with the a priori goal of having them desist in their identity based on the belief that some unnamed trauma is causing them to be transgender or homosexual, is conversion therapy.There is no evidence to support the efficacy of this approach. There is a substantial body of evidence supporting a more affirming one. Numerous recent peer-reviewed studies show that transgender youth who are supported in their gender identity by parents, schools, and their peers have significantly better mental health outcomes than those whose identities are rejected or stigmatized. Rejection includes efforts to change their gender identity, coercing them into suppressing it, or rejecting it altogether.
The vast majority of trans men who transition do not consider themselves heterosexual afterwards
One of the false narratives about adolescent trans youth is that they are predominantly young lesbians who are transitioning to male to appear straight, or because of misogyny inherent in our society. However, data from large-scale studies dispute that view. The largest survey of transgender men to date showed that only 23% of trans men identified as strictly heterosexual (i.e. attracted only to women). This line of argument also makes the dubious assumption that people think being transgender somehow makes one’s life easier. In the UK, a similar survey found that only 16% of trans men see themselves as heterosexual.Diagnostic criteria for childhood gender dysphoria specifically forbids diagnosing someone based on “mere tomboyishness in girls or girlish behavior in boys”
The ICD-10, the medical and mental health classification list of the World Health Organization, has this to say about diagnosing childhood gender dysphoria: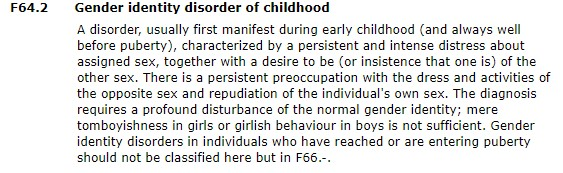
This is the current diagnostic criteria used by the most places outside the US. “Mere tomboyishness in girls” is not sufficient for a diagnosis of childhood gender identity disorder. Nor is mere ambivalence towards one’s gender sufficient: it requires a “profound disturbance”.
In the US, the DSM-5 is the standard for diagnosing gender dysphoria in youth. It too requires an insistent, consistent, and persistent cross-gender identity. Atypically gendered interests (e.g. playing with the “wrong” toys) and expression (e.g. what clothes a child prefers to wear) are insufficient for a gender dysphoria diagnosis. Thus, fears that somewhat gender non-conforming youth will be railroaded into transitioning are not supported by the diagnostic criteria put forward by the ICD or the DSM-5 today.
Transmasculine people can still have children after receiving testosterone
The use of exogenous testosterone in transmasculine people (trans men and nonbinary people) generally has the effect of suppressing menses. However, recent studies show that even transmasculine people that have been taking exogenous testosterone for years retain their fertility if they stop taking it. Indeed, their fertility rebounded to levels statistically indistinguishable from that of cisgender women of a similar age cohort. Permanent infertility is not one of common the side-effects of testosterone-driven gender affirmation. Nor does the research suggest that puberty blockers cause permanent sterility if the medication is discontinued.Transgender people who have medical treatment are less likely to suffer from anorgasmia or sexual aversion
The narrative that transgender people cannot have fulfilling sexual lives, or that transition prevents sexual enjoyment, is false. Transgender people who receive treatment for their gender dysphoria are less likely to suffer from sexual dysfunction than their untreated peers. Trans people who have undergone gender affirming surgery are more likely to enjoy sexual activity. The majority of transfeminine people who eventually undergo gender affirmation surgery report heightened orgasms. Transmasculine people typically report heightened sexual desire while on testosterone. While transgender individuals are more likely to suffer from sexual dysfunction than the general population, this seems to be due in great part to sexual aversion caused by unresolved gender dysphoria. The evidence at hand suggests that reducing gender dysphoria leads to a concurrent reduction in sexual aversion and increased in enjoyment of sex.Thus, the narrative that medical treatment for gender dysphoria sentences people to a life of sexual dysfunction is categorically false. Conversely, lack of access to treatment increases the long-term risk of dysfunction and dissatisfaction due to sexual aversion.
There is no basis to the assertion that parents believe having a transgender child is better than having a gay one
It is suggested that some parents see having an ostensibly “straight” child as better than having a gay one, and that they are then somehow pressuring their child into transitioning. This is implausible for so many reasons. First and foremost, people with hostile attitudes towards lesbians and gays usually also are hostile to transgender people, and often more so. Another study concluded, “homophobia is likely to always be the ‘best’ predictor of transphobia, and these two constructs probably share a common foundation.”Indeed, more families feel that being transgender is a worse outcome than being gay. A survey on LGBTQ youth found that the families of 64% of transgender youth, including non-binary youth, made them feel bad about their identities compared to 34% of cisgender LGBQ youth.
One would also have to assume that these theoretically homophobic (but not transphobic) parents would also somehow be able to coerce their child into being (or pretending to be) transgender. They would then have to get a referral, and then wait two years to get an appointment. The youth would then have to talk their way past therapists who see thousands of genuine trans youths every year, and yet produce very few false positives. All of this, taken together, seems highly implausible.
There has been an increase in the number of out transgender people globally for decades as societal acceptance, and access to care, improves
There has been significant growth in the number of people seeking treatment in Western nations for decades. This includes detailed data from the Netherlands, Sweden, and New Zealand. A meta-analysis of 17 studies from 1954 to 2014 found a statistically significant increase over time in the number of trans women and trans men presenting for evaluation and treatment.The increase should not be unexpected; the UK’s Gender Identity Research and Education Society (GIRES) published a report with grant funding from the Home Office in 2009, predicting growth in the UK’s treatment-seeking transgender population.
Studies over several decades have often seen higher ratios of transgender men to transgender women, or ratios that change over time
Godlewski (198There are cultural explanations as well. Kirrin Medcalf, the head of trans inclusion at Stonewall, noted of the difference between trans boys and trans girls in the system:
I think because parents and society are more tolerant of children who are assigned female at birth behaving masculine. Those assigned male at birth and presenting feminine behaviour is still much more taboo, and parents are less likely to act on that. Children also pick up on that and come out later.
There is no evidence that youth find it easier to come out as trans rather than LGB
The American Center for Disease Control (CDC) data show that 11.8% of adolescent girls identify as lesbian or bisexual. Only 1.9% of all adolescents identified as transgender. Even if all those are trans boys, it still does not support the assertion that youth find it far easier to come out as transgender. The roughly 10-1 (or greater) ratio between cisgender LGB people, and trans individuals in data sets has held true for close to a decade. In 2011, the Williams Institute at the University of California Los Angeles found that 3.5% US adults identified as LGB, and that 0.3% identified as transgender. Occam’s razor suggests that as society has become more accepting, more people are willing to explore their gender and sexual orientation and come out as a result.Conclusions
As evidenced above, there are many misconceptions surrounding the medical care of trans youth. The scientific misinformation spread through mainstream media is far from benign as trans youth throughout the U.S. are losing access to potentially life-saving care. Laws targeting access to care are not grounded in reputable science and should not guide the care of this marginalized population.Authors
Brynn Tannehill
Brynn Tannehill is originally from Phoenix, Ariz. She graduated from the Naval Academy with a B.S. in computer science in 1997. She earned her Naval Aviator wings in 1999 and flew SH-60B helicopters and P-3C maritime patrol aircraft during three deployments between 2000 and 2004. She served as a campaign analyst while deployed overseas to 5th Fleet Headquarters in Bahrain from 2005 to 2006. In 2008 Brynn earned a M.S. in Operations Research from the Air Force Institute of Technology and transferred from active duty to the Naval Reserves. In 2008 Brynn began working as a senior defense research scientist in private industry. She left the drilling reserves and began transition in 2010. Since then she has written for OutServe magazine, The New Civil Rights Movement, and Queer Mental Health as a blogger and featured columnist. Brynn and her wife Janis currently live in Xenia, Ohio, with their three children. Follow Brynn Tannehill on Twitter: www.twitter.com/BrynnTannehill
David Gorski
Dr. Gorski's full information can be found here, along with information for patients. David H. Gorski, MD, PhD, FACS is a surgical oncologist at the Barbara Ann Karmanos Cancer Institute specializing in breast cancer surgery, where he also serves as the American College of Surgeons Committee on Cancer Liaison Physician as well as an Associate Professor of Surgery and member of the faculty of the Graduate Program in Cancer Biology at Wayne State University. If you are a potential patient and found this page through a Google search, please check out Dr. Gorski's biographical information, disclaimers regarding his writings, and notice to patients here.
AJ Eckert
Dr. AJ Eckert, D.O. (they/them) is Connecticut’s first out nonbinary doctor, Medical Director of Anchor Health’s Gender and Life-Affirming Medicine (GLAM) Program, and Assistant Clinical Professor of Family Medicine at Frank H. Netter MD School of Medicine at Quinnipiac University. Dr. Eckert has been involved in LGBTQ healthcare for over fourteen years with seven years’ experience as a provider of primary and preventative care and gender-affirming services, including hormone treatment and puberty blockers. Dr. Eckert hosts Queering Health with Dr. E, Anchor Health’s bimonthly YouTube and IGTV show, which focuses on demystifying LGBTQ healthcare and promoting the wellness of queer people through open discussions, stories, interviews, and more.
Source (Archive)