- Joined
- Sep 9, 2021
Simon Sun and company discuss their desire to test GAT in rats. Paper here.
Abstract:
Here is a second paper on the 'gender binary cycle'. It mostly complains of gender norms so I'll post relevant topics here.
Not to worry, their solution is just to have people read theory:
There is a bit on human brains that is accurate; while there is no 'male' or 'female' brain per se, they do exhibit certain differences that you can say which one is male or female. Troons love using the brain argument so it is nice to see it get spat in their faces (again).
They complain about gendered language:
We're the same but also different but don't say that we are different because that's bigotry:
Gotta change it as the base level, yo:
Blank Slate theories never serve anyone well. Look at Lebron's 'I Promise' school for proof.
Abstract:
Oh I cannot imagine there'd be any ulterior motive in this, no sir.We have recently proposed experimental design guidelines and areas of study for preclinical rodent models of gender-affirming hormone therapy in neuroscience. These guidelines also apply to any field subject to the influences of gonadal steroid hormones, including metabolism and growth, cancer, and physiology. This perspective briefly describes our suggestions for these fields. Studying the effects of exogenous steroid hormones will have translational benefits for the community. We also discuss the need for equitable practices for cisgender scientists who wish to implement these guidelines and engage with the community. It is necessary that community-informed practices are implemented in preclinical research to maximize the benefit to transgender, nonbinary, and/or gender diverse (TNG) healthcare, which is currently in jeopardy in the United States, Europe, and across the globe.
He references another troon, Jules Gills Peterson, who wrote a seminal book on the trans child. He also has another book published this year, 'A Short History of Trans Misogyny', which will surely have a place in the 'Trans Made Media' thread.The gonadal steroid hormones estrogen, progesterone, and testosterone have been used by people for sex/gender transition since their initial discovery approximately a century ago. In the decades since, the use of these hormones as gender-affirming hormone therapy (GAHT) became widespread among transgender individuals for biomedical sex/gender transition (for historical reviews of hormonal and other treatments of transgender children and adults, see [1].
"We don't know but give us the hormones anyways or else we'll kill ourselves."Although the precise influences of gonadal steroid hormones on mental health are unclear (and likely dependent on social and environmental context), GAHT is clearly associated with improvements in mental health—regardless of formulation [2].
I guess all those suggestions never panned out, eh? Here I thought none of these 'sex hormones' were specific to a certain sex. Glad to see Sun did a 180 on it when it applies to his special group.Nevertheless, there remains a dearth of research into the mechanisms by which GAHT improves mental health outcomes. This lack of research is used by anti-transgender activists to justify discriminatory practices and limit access to or outright deny care. An increasing number of states in the USA have enacted new laws and regulations limiting the ability of transgender children to access GAHT, which de facto forces some children to medically detransition [3]. As of June 2023, the number of states limiting access to care has increased to 20. In some states, implementation of laws banning GAHT for children also result in de facto bans for adult GAHT [4]. The current sociocultural and geopolitical moment, in combination with the difficulty of mechanistic neuroendocrine studies in humans, points to an urgent need for well-designed preclinical studies.
Experimenting on poor mice to get those magic girl juice drugs. They deserve better.To address this exigent issue, we recently published a review outlining how to best design such studies [5]. Studies on the influence of estrogen-based GAHT (E-GAHT)/testosterone-based GAHT (T-GAHT) on physiological or neurological processes should be evaluated on whether “classic” endocrinological techniques (gonadectomy with surgical pellet implantation) or new GAHT models are most appropriate. In our review, we proposed best practices for experimental design that recapitulate the human experience of GAHT, such as comparing intact rodents with gonadectomized rodents, applying steroid replacement to both, and treating with androgen receptor blockers commonly used in E-GAHT. This work should focus on the needs of transgender populations. Here, we provide a brief overview of our recommendations for preclinical rodent models of GAHT and emphasize how this research should be conducted to address the material health needs of transgender populations.
If you recall Sun's previous paper, he argued that there was no such thing as 'male' or 'female' sex hormones, and that the gonads didn't really play a role in their development; or, at the very least, they do not make a sexed body. But when it comes to demanding hormones for trans people, he throws that out and takes the bioessentialist position he so hates.Receptors and Gene Expression
Gonadal hormones (estrogens, progestins, and androgens) exert their effects by acting as ligands to their cognate receptors. The most well-studied of the hormone receptors are the canonical nuclear receptors: estrogen receptor alpha and beta (ERα, ERβ), androgen receptor (AR), and progesterone receptors (PR-A, PR-B). These receptors are expressed at varying levels throughout the brain, with notably denser expression in subcortical regions important for social behavior, stress responses, metabolism, mood/affect, memory, and cognition. Therefore, understanding the mechanisms by which gonadal hormones influence these aspects of neural function is fundamental for improving GAHT.
"Sex doesn't exist, but it does, and we need specific pathways to get personalized healthcare for a group that wants to be something that doesn't exist."Nuclear hormone receptors regulate gene expression to drive changes in neural circuit wiring, synaptic strength, and neural activity. When bound with their ligand, these receptors interact with the genome, acting as transcription factors and modifying chromatin profiles [6]. Recent research indicates that sex variability in neuronal gene expression is reliant on the acute hormonal environment, suggesting a potential mechanism by which GAHT can flexibly influence neuronal function throughout an individual's lifetime [7]. Additionally, gonadal hormones can act on nonneuronal populations, including microglia and astrocytes and may contribute to the mental health benefits associated with GAHT. Future research that links hormone-dependent neuronal activity changes with hormone-dependent gene regulation could reveal molecular pathways for personalized GAHT.
You know that if they found anything bad resulting from their little titty skittles that it would never see the light of day. These drugs are straight miracles to them; they ain't never giving up that faith.Membrane-bound hormone receptors are found on both the plasma membrane and the surface of organelles. Once ligand-bound, these receptors are often thought to initiate molecular cascades, leading to changes in cell function and behavior. The timescale of action is hypothesized to lead to parallel mechanisms of intracellular action in concert with nuclear receptor activation. Future research on GAHT could illuminate the interplay between membrane-bound receptors and nuclear receptors and interrogate how each receptor-type distinctly affects cellular function in multiple tissue-types.
They don't know, yet they demand kids get these 'treatments' anyways or else they'll die. This is purely an experimental procedure where they don't even have a solid percentage of success. The few studies we do know of show neurological degeneration in puberty blocked kids, but troons always throw a fit over it. Troon scientists acting as gatekeepers will prevent the facts from ever getting out.Cognition/Memory
Cognition, memory, and learning are influenced by gonadal hormones, and many of the brain regions involved in cognition express steroid receptors. However, evidence that estrogen replacement therapies can protect against cognitive decline remains controversial. Studies in cisgender humans partially support the hypothesis that steroids influence cognition and memory in older adults across sex. The influence of GAHT on cognitive measures in transgender, nonbinary, and/or gender diverse (TNG) people—in youth seeking to delay puberty or in older TNG individuals with years of GAHT—remains largely unknown. More clinical and preclinical studies are needed to assess the mechanisms of GAHT on cognition and memory and the interactions of GAHT and social/minority stressors in young and aging TNG populations.
They're using the minority stress model again. And yet, despite allegedly being victims of the worst genocide ever, trans people still display higher rates of narcissism and BPD than other populations. Very strange behaviour, we should study it sometime.Mood/Stress Disorders
Hormonal milieus interacting with multiple brain regions lead to differences in the etiology, symptomology, and effectiveness of treatments for mood and stress disorders. Evidence that GAHT alters stress reactivity in clinical settings suggests that it has direct actions on stress circuitry, which may impact the mental health needs of individuals treated with GAHT. However, studies examining GAHT-associated mental health run the risk of pathologizing GAHTs. Therefore, we propose 2 lines of inquiry to pursue through animal models of mood and stress disorders. The first compares GAHT-treated animals to untreated controls, which may identify the direct action of GAHT on mood and stress-related brain regions. The second examines the mental health outcomes using animal models of mood and stress disorder by comparing GAHT-treated animals differentially exposed to an additional variable. Gender-based discrimination and perception of the contemporary geopolitical climate are related to elevated biomarkers of allostatic load in transgender populations. Such factors can be conceived as chronic psychosocial stressors; as such, particular focus should be given to rodent models of chronic psychosocial stress.
Very encouraging: 'we don't know the long terms effects of this, but we will relentlessly support it because we care more about our identity group than anyone else.'Metabolism
Although steroidal hormones and their effects on general metabolism and physiology are historically well-studied, much remains to be studied about GAHT and its long-term outcomes on growth, overall metabolism, and bone health.
We already have some. Transwomen get fat, transmen gain some muscle and then lose it and get fat, and they still retain their sex based fat disposition. Nature is truly a TERF.Both estrogens and androgens are thought to regulate feeding behaviors, homeostatic control of thermoregulation, and overall body mass. However, as few studies have examined the effects of E-GAHT and T-GAHT on long-term body composition and growth, we propose preclinical studies to understand how varying regimens of GAHT lead to changes in body weight and the localization of fat accumulation before and after GAHT.
And when they get the results they don't like, they'll flush it down the memory hole. Good to see they're coming to the same conclusions as the researchers over at WPATH.These studies would allow for further tailoring of GAHT regimens to increase satisfactory transition outcomes in TNG populations. Additionally, bone health is thought to be regulated in part by circulating steroidal hormones. Age-dependent bone loss is partially attributed to a dysregulation of gonadal steroids. To address this, we propose longitudinal studies that examine the effects of GAHT on bone health in older TNG individuals and the maintenance of bone growth in young and middle-aged TNG individuals.
That's very encouraging, tell me more.Cancer
While much of our focus has been on neurobiology, our models can be easily applied to other endocrine-sensitive physiological and pathophysiological processes, such as cancer. While much has been written about health disparities in the TNG community in the context of cancer, the influence of GAHT on the prevalence of or risk for endocrine cancers is understudied.
So they don't know and admit they're running on a gambit with this. They don't care because muh trans rights comes first.Furthermore, the mechanisms underlying these effects can only be postulated due to the lack of preclinical studies in animal and cellular models. Questions that can be addressed by the proposed models include both short-term and long-term treatment with both E-GAHT and T-GAHT in young adult and aged rodents, activation of cellular processes by both treatment types on ER/PR-positive breast cancer cells, the influence of E-GAHT on prostate cancers, and the long-term effects of pubertal delay on endocrine cancers, including intestinal and reproductive cancers.
"Include us in your work or else."Conclusions
We must recognize that animal GAHT models are limited in their ability to fully study the uniquely human experience of gender-affirming treatments. However, these models can improve our knowledge of how GAHTs influence physiological and neurological processes. It is imperative to understand that GAHT and the social stressors discussed could have reciprocal influences on their actions and should be individually and synergistically studied. There remain significant barriers to healthcare and to STEM careers for TNG people, which are amplified by current political decisions. As such, studies using the proposed preclinical models of GAHT must incorporate collaborations with TNG community members, either in the lab or through community outreach.
As mentioned ITT, Sun and colleagues don't have any meaningful solutions aside from 'do all these batteries of tests to prove something isn't binary when it will clearly come down to being binary.' To them, variations with a sex are variations OF sex, and that attributes within A clearly cannot remain within A and so on and so forth.As transgender, nonbinary, and gender diverse identities are increasingly common, the prevalence of binary classifications significantly hinders meaningful research, particularly when applied to the human condition.
Oh, I'm very pleased. Surely they'll get all these neat result and not burn them once they don't get what they want, right?The TNG community has identified GAHT research priorities for GAHT [8] to ensure study outcomes and interpretations that align with TNG needs and experiences. Our proposed preclinical GAHT mouse models can create beneficial relationships between science/healthcare and the TNG community, but only when appropriately applied and with direct involvement of the TNG community.
Here is a second paper on the 'gender binary cycle'. It mostly complains of gender norms so I'll post relevant topics here.
I'm sure it'll stick to inane bullshit like this, right? No, it gets worse.Gender ideology is defined as ‘individuals’ level of support for a division of paid work and family responsibilities that is based on the notion of separate spheres' [9, p. 87]. The beliefs associated with gender ideology reflect the endorsement (or lack thereof) of a binary separation of family versus work responsibilities along gender lines, and the acceptance of the gender hierarchy resulting from it. For example, research on gender ideology has asked respondents to report whether they agree or disagree with statements about separate, and gendered, responsibilities of women and men (e.g. ‘A man's job is to earn money; a woman's job is to look after the home and family’; [10]); and about justification of men's privilege (e.g. ‘It is more important for a wife to help her husband's career than to have one herself’; [11]). To the extent that support for such items is high, we refer to the gender ideology as non-egalitarian.
Notice genetics is never mentioned. Our non human primate cousins act in similar manners, even when they don't have a concept of gender: males are more aggressive, females tend to be more nurturing (and even like playing with dolls). So this is just your typical gender studies paper.There are differences between women and men in many life domains. The lay theories that people hold regarding the sources of these differences fall into two main categories. According to the first, gender differences are a result of the different way people think about and act towards women and men—a socio-cultural theory/explanation. This explanation is consistent with accounts that view gender ‘as an emergent feature of social situations’ rather than a property of individuals [24, p. 126]. According to the socio-cultural explanation, girls and boys, and later on men and women, are being treated differently by others in a way that creates and reinforces gender differences. Examples of such treatment are teachers who expect boys to be better than girls at maths (e.g. [25]), parents who expect their children to avoid toys that ‘belong’ to the other gender (e.g. [26]) and media portrayals that routinely underscore women's sexuality [27].
Ah, there it is. The Blank Slate view of 'genes don't matter unless I want them to.' It's like the authors are shocked at this revelation; indeed, they act further shocked when normies agree with those claims:Another way people understand gender differences, which we term a biological-essentialist theory/explanation, is to view them as stemming from biological differences between men and women. According to this explanation, owing to their different biological make-up, men and women have distinct ‘essences’ and thus are predisposed to differ mentally and behaviourally. At the core of this explanation are the genetic and hormonal differences between females and males, viewed as the determining factors of masculinity and femininity [28–31]. Such a biological-essentialist lay theory considers differences between women and men as predetermined and immutable, and views gender as a binary, such that men and women are viewed as different ‘kinds’.
It is true, men and women are different. But the authors take great umbrage with this, and go on to say math abilities in men vs women are not due to genetics, but sexist teachers:A recent poll conducted among a nationally representative sample of 4573 adults in the USA [34] found that the majority of respondents agree that men and women ‘are basically different’ on domains related to expression of emotions, parenting style, interests and abilities. The majority of men further indicated that the differences are mostly based on biology (61% indicated biological differences explain why men and women have different strengths in the workplace, and 58% believed biology accounts for gender differences in parenting). The majority of women viewed gender differences as based on societal expectations, though 39% believed biology explains gender differences in parenting and 35% believed biological differences explain gender differences in workplace-relevant strengths.
Men occupy both tail ends of the bell curve, meaning they are more retarded and more are to be found in the high brilliance section. This does not mean women are stupid.Demonstrating downstream consequences of such effects, women who were provided with a biological-essentialist account of gender differences in maths (i.e. men perform better owing to genes on the Y chromosome), performed worse on a maths test than women provided with a socio-cultural explanation (i.e. that teachers have biased expectations favouring men; [37]).
Not to worry, their solution is just to have people read theory:
On differences between males and females regarding hormones:For example, greater belief in the deterministic role of biology in human development was associated with more sexist beliefs (e.g. believing that progressive gender policies are unnecessary; [42]; see also [43]) and with opposition to transgender people's rights [44]. Gender essentialism also predicted greater support for gender discriminatory practices and greater perceived fairness of gender inequality [45]. These findings were corroborated by experimental evidence. People who were randomly assigned to read a biological-essentialist view of gender (versus a social–cultural view) were less likely to support rights of women and of transgender people [46]. Similarly, reading theories that provide a biological-essentialist view of gender differences increased people's acceptance of gender inequality [47]. A recent study further showed that exposure to a biological explanation of gender differences (versus a social constructionist explanation or no explanation) increased endorsement of essentialist views which led to decreased recognition of gender discrimination [48].
Yes, we know. We also know men produce far more testosterone than women and women produce more estrogen than men. You also cannot argue this while demanding that trans people get 'gender affirming hormones' that associate with the sex you say they don't.In contrast with popular beliefs, endocrinology research reveals that humans do not possess one of two sets (‘female’ or ‘male’) of sex-related hormones. Rather, hormones that are considered ‘female’ (oestrogen and progesterone) and those considered ‘male’ (e.g. testosterone) are present in both men and women as they are produced by both ovaries and testes as well as by additional tissues that are present in all bodies (for a review, see [49]).
The paper they are referencing is about women on oral contraceptives. The testosterone levels in men and women differ immensely, and you can see it in any paper discussing physiology. Another case of authors not reading the papers they cite.
The paper they are referencing has a graph on page 7 showing the overlap. They are nowhere near equal.Although testosterone levels are higher on average in men than women, the difference is smaller than widely believed, does not exist at all stages of life and the distributions of testosterone levels of men and women show considerable overlap [52].
That doesn't mean anything. Women having higher testosterone does not make them men, nor does it mean their T levels are on their level. This is a tired old argument that needs the Old Yeller treatment.Moreover, the levels of sex-related hormones vary widely within individuals, changing across the lifespan as well as in response to internal and external conditions, including gendered behaviours [53,54]. For example, sexual thoughts increase testosterone levels in women [55] and nurturing parenting behaviours decrease testosterone in men [56]. Thus, gender differences in levels of sex-related hormones do not conform to a fixed and binary conceptualization [53,57].
There is a bit on human brains that is accurate; while there is no 'male' or 'female' brain per se, they do exhibit certain differences that you can say which one is male or female. Troons love using the brain argument so it is nice to see it get spat in their faces (again).
They complain about gendered language:
Denying genetic influence again:Gender is routinely used as a label and as a sorting dimension. By gender-based labelling, we refer to the marking of an individual as a girl or boy, as a woman or a man. Language is central for labelling. People constantly use gender labels in everyday language (‘girls’ or ‘boys’, ‘men’ or ‘women’), often when unnecessary (e.g. teachers who greet their classrooms with ‘Good morning, boys and girls’ rather than ‘Good morning, students’; see [70]). Gendered labels are also used in specific domains such as occupations (e.g. actress, or soundman) and are, in some languages, routinely used to describe inanimate objects (e.g. a fork is male and a spoon is female in Hebrew; see [72]). Gender labelling is enacted not only through language. For example, throughout history, gender-differentiated dress was legally mandated in many public settings, including schools and workplaces [73], and norms continue to dictate that men and women differ in their dress and use of accessories.
The kid would be right assuming it is in the child's genes to act that way. Over 80%, in fact.For example, studies reveal that essentialist accounts of social categories, including the perception that differences between groups are biologically innate, are more common than extrinsic accounts [86]. Thus, a child might conclude that a peer who acts in a certain way must have been born that way, because no alternative explanations are salient (see [87]).
We're the same but also different but don't say that we are different because that's bigotry:
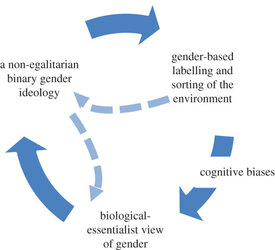
On two types of humans:The second additional path indicates that a non-egalitarian gender ideology can drive a biological-essentialist view of gender differences (dashed line on the left side of the model in figure 1). A biological-essentialist view of gender can be recruited by people who endorse a non-egalitarian gender ideology in order to provide justification and validity to their ideological stance. The belief that differences between men and women are inherent, meaningful and inevitable renders role-separation and power disparities logical and justified [41]. In support of this feedback loop, research shows that the more people are motivated to sustain group-based hierarchy, the more likely they are to endorse essentialist views of gender [45].
You being mad won't stop the research from being done.Early portrays of women described them not only as biologically distinct from men, but also as inferior on almost every aspect of human functioning [92]. The notion that males' brains are designed to facilitate processes that are fundamentally different than those facilitated by females’ brains still prevails, and many studies are devoted to detecting sex differences in brain structure and function. The results of such studies are often interpreted, in both scientific and popular contexts (e.g. press releases, traditional news media), through the binary framework—the differences are overemphasized (in terms of their size and significance) and assumed to add up within individuals to create two types of humans [62,94,95].
Nice little contradiction there. Not that many would notice.While today scientists would not go on to claim that women are inferior to men, their portrayal of sex differences in the human brain often aligns with gender stereotypes. For example, a large study of connectivity in the human brain concluded: ‘Overall, the results suggest that male brains are structured to facilitate connectivity between perception and coordinated action, whereas female brains are designed to facilitate communication between analytical and intuitive processing modes' [96, p.823]. This claim was made even though only several dozen connections, of the over 9000 assessed, showed moderate sex/gender differences (Cohen's d ∼ 0.3; [97]), and the authors did not test whether the differences add up to two types of connectivity patterns. As reviewed earlier, a later study revealed that this is not the case, as most brains possess unique mosaics of connections, some with the strength more common in women and others with the strength more common in men [58].
Gotta change it as the base level, yo:
On tard wrangling:The second point of intervention is challenging the biological-essentialist perspective, either by refuting its claims that gender differences are immutable and add up to two kinds or by providing an alternative, non-essentialist explanation, to gender differences. As described above, even a short text that provides adults with a social account of gender differences can reduce the use of gender stereotypes and promote a more egalitarian outlook on gender roles and relations.
Might as well add the figure they used for the paper:The same approach can be harnessed for dealing with gender differences that are assumed to be innate. For example, if boys are assumed to lack in empathy or to be aggressive as a result of exposure to hormones in utero, then appropriate social measures (e.g. educational training) should be taken to increase their empathic and inhibitory abilities, as would have been done if their empathic deficit or aggressive tendencies were attributed to a contextual factor (e.g. maltreatment on part of parents). That this is not the approach taken in relation to biological explanations of gender differences is yet another testimony to the tight relations between these explanations and gender ideology. The alternative approach we suggest can be facilitated by raising awareness to the tendency to celebrate, rather than challenge, gender differences, and to the costs of such tendency: the perpetuation of gender inequality and the costs to people's fulfilment of their full potential [98].
Blank Slate theories never serve anyone well. Look at Lebron's 'I Promise' school for proof.

















